Testing for hepatitis C as a sexually transmissible infection: understanding health practitioners’ knowledge and attitudes
Testing for hepatitis C as a sexually transmissible infection: understanding health practitioners’ knowledge and attitudes
HIV Australia | Vol. 11 No. 2 | July 2013
SOENKE TREMPER and GUY HUSSEY outline survey results that give insight into GPs’ perspectives on hepatitis C transmission among HIV-positive men who have sex with men.
Background
In 2011, the Victorian Department of Health noted an increase in diagnoses of hepatitis C (HCV) virus infections among men who have sex with men and who live with HIV.1
In early 2013, Living Positive Victoria convened a reference group to assist in the development of health promotion initiatives that seek to lower the risk of HCV infection among HIV-positive men who have sex with men.
During the first reference group meeting in March 2013, the group identified that general practitioners (GPs) who provide care for HIV-positive men who have sex with men may have particular perspectives about these men’s risk behaviours, knowledge, and attitudes regarding HCV prevention techniques.
The reference group decided, as a first step, to develop a survey that identifies the GPs’ knowledge and attitudes regarding HCV transmission among HIV-positive men who have sex with men.
General Practice Victoria (GPV) developed a brief electronic survey, which was reviewed by Living Positive Victoria’s health promotion team.
The survey was not conducted as a formal research project, but rather as a means to inform project development.
Sample selection
The survey was sent to a total of 72 health practitioners, consisting of: Victorian HIV s100 authorised general practitioners (34), general practitioners (5), sexual health physicians (12) and infectious diseases physicians in Victoria (21).
GPV used two email groups, maintained by its Sexual Health, HIV, Hepatitis Education (sh3ed) program, to disseminate the link to the online survey.
Email group one: ‘HIV s100 GPs’
This group consisted of GPs and sexual health doctors with a specific interest in HIV. It should be noted that this group includes all Victorian HIV s100 authorised GPs, and is therefore very highly representative of the target population (Victorian HIV s100 authorised GPs).
Email group two: ‘HIV ID Clinics’
This group consisted of infectious diseases physicians and some registrars working across the main Victorian infectious diseases outpatients clinics.
This list was included to understand if there is a difference in knowledge and attitudes depending on care setting.
The survey
A total of 13 responses to the survey were received. At 18% (13/72), the response rate was low, and would generally be considered suboptimal in a formal research environment; however, the clinicians who participated in this informal questionnaire represent the majority of high caseload primary care centres and sexual health clinics.
While information gained from this survey should not be generalised, it does provide useful insights into the knowledge levels, attitudes, beliefs, and practices of healthcare professionals working a high caseload setting in Melbourne.
GPs who were HIV s100 accredited made up the majority of survey respondents (53.9%), followed by infectious diseases physicians (30.8%) and sexual health physicians (15.4%).
No sexual health physicians who work in Melbourne Sexual Health Centre’s Green Room (HIV referral clinic) participated in this survey.
HCV awareness – impact on practice
The majority of respondents (84.6%) said they were aware of the increase in diagnoses of HCV infections among HIV-positive men who have sex with men noted by the Victorian Department of Health in 2011.
Of the eleven respondents who were aware, eight stated that this awareness changed the way they practise. The two participants who were not aware requested further information, which was provided via follow-up email through GPV.
Table 1 shows individual responses of the eight GPs who changed the way they practise, or why they deemed no change was necessary.
Table 1
| Change in practice due to hep C awareness |
|---|
| Annual HCV screening in HIV-infected patients and discussion and passing on info to patients [regarding] potential sexual transmission |
| Counselling HIV-positive MSM about this risk and attention to HCV screening as part of STI screening in those at risk |
| I have always included HCV screening in the routine STI screening in my patients. When I talk to them about risks of STI transmission I include HCV |
| Discussed this with my [patients], particularly my HIV pos [patients], encouraged condoms with casual partners |
| Advise all patients, discuss practices and risk |
| More frequent testing of hep C in HIV-positive men More likely to have a discussion re: high risk sexual practices and IVDU [intravenous drug use] amongst HIV-positive men. |
| [No], already routinely screening HIV-positive men who have sex with men for hep C |
| Patients have regular LFTs [liver function tests] and should have repeat HCV screening |
Responses indicate that these participants felt that they have integrated HCV testing into their routinely undertaken panel of tests for HIV-positive men who have sex with men.
Some indicated that they had done so before the noted increase in diagnoses.
Twelve of the 13 respondents stated that they had integrated HCV testing into their routinely undertaken panel of tests for HIV-positive men who have sex with men.
These responses suggest that the vast majority of participants regularly test for HCV, driven by perceived risk strata rather than event driven testing.
Testing for sexually adventurous men
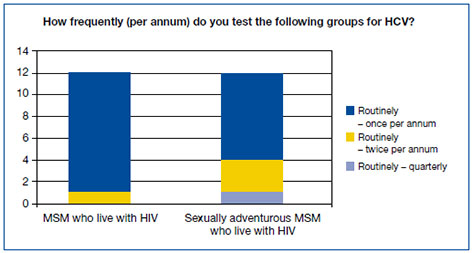
Although eleven of 13 respondents were aware of an increase in diagnoses of hepatitis C among HIV-positive men who have sex with men, only four participants tested sexually adventurous men at least once every six months, in accordance with the National Hepatitis C Testing Policy. Eight of 11 (72.7%) participants did not adjust frequency of hepatitis C testing with increasing risk profile. (See Figure 1.)
Figure 1: HCV test frequency
This suggests that these participants either:
- set an inappropriate testing frequency for a high risk group and applied this to lower risk groups; or
- did not see value in testing more frequently despite increased risk; or
- were not aware that there is increased risk depending on sexual practices; or
- use other strategies that this survey did not appropriately cover; or
- experience other barriers that this survey did not cover.
To understand what participants understood ‘sexually adventurous’ to mean, and how this meaning may influence HCV testing, participants were asked to provide a definition. Table 2 provides all ten answers received.
Table 2
| Who qualifies as sexually adventurous MSM? |
|---|
| SOPV [sex on premises venues]/group sex/fisting |
| It’s not a term I use, but the people I consider most at risk for dual HCV acquisition are those who are having unprotected RAI [receptive anal intercourse], particularly those who have many/ anonymous partners and/or those who combine sex with drug taking and/or those who fist etc. |
| UAIC [unprotected anal intercourse] with multiple partners, particularly if blood/trauma during sex |
| Higher number partners, group sex, crystal users |
| Fisting, blood sports |
| Large no of partners, >10 per quarter, group sex, toys, travel to high risk areas |
| Frequent attenders of SOPV Those engaging in fisting Those engaging in sex parties/multiple partners at a time Those who practice unsafe sex with recreational drugs involved |
| All patients having three or four monthly LFTs [liver function tests] as well as annual Hep C. Sexually adventurous includes people in open/non monog [non-monogamous] relationships/ casual sex partners/BDSM [bondage, discipline, sadomasochism]/blood letting/IVDU and meth as part of sex |
| ‘Someone who has more sex than their doctor’ |
| MSM who self-identify as regularly having more than one partner |
With few exceptions, participants’ free text answers suggest an understanding that HCV transmission occurs where blood is present or where people engage in abrasive practices in or around sex.
Drugs appear to be referred to in two ways: as stimulants that reduce risk awareness, and as a mode of infection (sharing of injecting equipment).
Some of the answers centre on particular practices whereas others focus on frequency of sex; others offer a mix of practices and frequency.
None of the answers identify possible drivers of behaviours. The threshold for who is or is not considered sexually adventurous varies considerably, from ‘regularly having more than one partner’ through to ‘fisting, blood-sports’.
Health promotion issues
Lastly, participants had the opportunity to share anything else that came to mind. Two comments were received:
‘I find that many [patients] aren’t worried about Hep C as they perceive it is curable, or they perceive themselves as low risk even when having regular unprotected sex.’
and
‘I think the message is getting to them reasonably rapidly.’
There were differing opinions about penetration of health promotion messages between these two participants.
The first suggests that patients who have unprotected sex regularly don’t perceive themselves to be at risk, whereas the second suggests that information about HCV as a sexually transmissible infection is being received.
A key question to answer is which communities or groups are receiving messages.
It is possible here that the two respondents are referring to two groups at differing risk (e.g., men who have sex with men vs sexually adventurous men who have sex with men and who live with HIV).
These two comments reflect a view that some HIV-positive men who have sex with men are aware of the risk (higher perceived susceptibility), but ignore it since HCV is curable (lower perceived seriousness).
This issue is highly relevant to development of health promotion regarding HCV targeting sexually adventurous HIV-positive men.
Conclusion
Survey responses indicated that most participants believed either that their practice already accommodated for hepatitis C as a sexually transmissible infection in at-risk individuals, or that they had adjusted their practice in light of the noted increase in diagnoses.
Most participants (12/13) test HIV-positive men who have sex with men for hepatitis C regularly (once per annum), regardless of whether they are considered sexually adventurous or not.
Of note, there is a gap between what participants identify as appropriate testing frequency for sexually adventurous men (annually) and what the National HCV Testing Policy recommends (every six months).
There is also diversity in which behaviour qualifies as sexually adventurous: the threshold for who is or is not considered sexually adventurous varies considerably, from ‘regularly having more than one partner’ through to ‘fisting, blood-sports’.
The identified inconsistencies and the gap between participants’ practices (based on their attitudes and beliefs) and current policy/guidelines need to be addressed. This reflects a lack of resources for healthcare providers.
Resource development is needed to:
- position hepatitis C as a sexually transmissible infection in HIV-positive men who have sex with men, and
- increase understanding of risk associated with particular sexual practices.
The survey results suggest that healthcare providers’ beliefs and attitudes towards sexually adventurous men – and understanding of the sexual practices they engage in – need to be better understood, in order to ensure that providers change practice with respect to identification of risks and adjusting clinical care accordingly.
As the identified gaps seem to be based on attitudes and beliefs rather than a pure clinical/medical knowledge gap, GPV would strongly support a joint community and GP led campaign that seeks to improve awareness of HCV risk associated with particular sexual practices, with resources developed by healthcare professionals and community representatives, working together in partnership.
References
1 Mahoney, A., Donnan, E., Lester, R., Doyle, J., Knox, J., Tracy, S., et al. (2013). Beyond injecting drug use: investigation of a Victorian cluster of hepatitis C among HIV-infected men who have sex with men. Medical Journal of Australia, 198(4), 210–214. DOI:10.5694/mja12.10556
2 Australasian Society of HIV Medicine (ASHM). (2012). National hepatitis C testing policy. ASHM, Sydney. Retrieved from: http://testingportal.ashm.org.au/hcv
Soenke Tremper is the team manager for population health at General Practice Victoria.
Guy Hussey is Senior Programs and Policy Officer at Living Positive Victoria.

